Auto logout in seconds.
Continue LogoutThe health care industry has made a critical decision. By and large, leaders have decided that health equity is central to their mission as health care organizations—or at least, it should be. The past two years ushered in unprecedented experimentation and investment in health equity as many organizations waded into these waters for the first time.
That experience solidified for leaders just how daunting the path is ahead. Many don't feel ready. And most organizations still grapple with conflicting incentives that put health equity goals at odds with other strategic priorities.
2 potential paths for the future of health equity
This dynamic has positioned health care leaders at a crossroads. And the decisions that each organization makes will set the course for health equity. There are two possible futures:
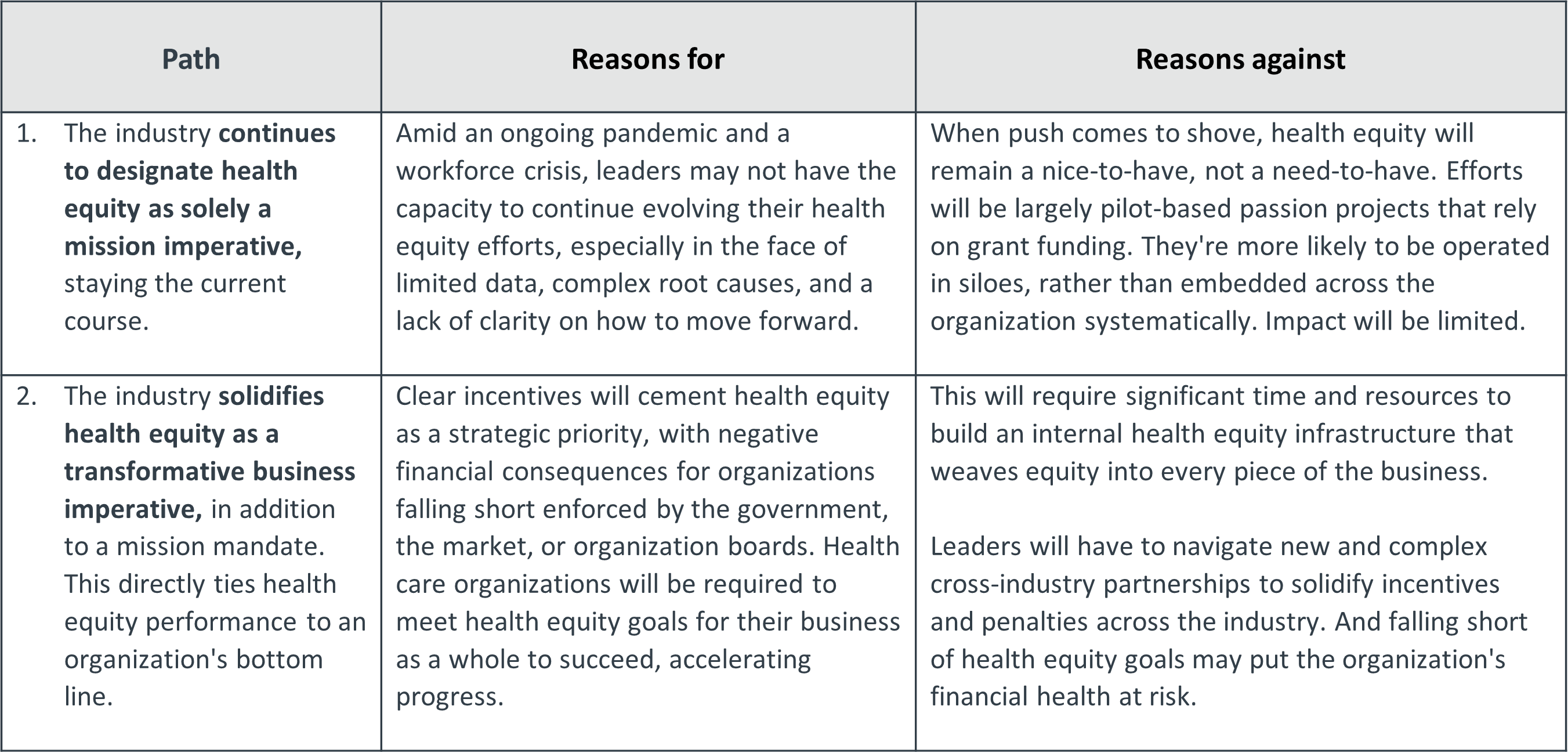
Until recently, we would've been willing to bet that the mission imperative focus of Path 1 above was the most likely to come to bear. That's changed for a few reasons.
First, the federal government has kept the industry's eyes on health equity, even in the face of competing priorities. President Biden's administration has demonstrated consistent interest in advancing equity, ranging from declaring racism a public health threat to opening up new funding opportunities to redesigning CMS programs with equity at the core. Notably, the administration has also been able to work with bipartisan partners in Congress to advance these goals.
But arguably the most interesting development goes beyond action in the public sector. Plans and employers have started to coalesce around a new tactic: holding provider organizations accountable for delivering equitable care by weaving equity into quality metrics.
Just as providers already receive payment bumps for meeting certain quality metrics and penalties for falling short, providers in these new contracts will now also be accountable for any gaps between demographic groups. It's no longer sufficient for performance to be good on average if there is variation under the surface. BCBS of Massachusetts has led the charge, but other entities quickly followed—including Morgan Health and CMS with its new ACO REACH model.
Integrating equity into quality is promising—but will it deliver?
This strategy is a brand-new approach for advancing health equity and is still in the early stages. It could unfold in different ways:
- Optimistic outlook: Assuming more organizations adopt the model, this approach could mark a turning point in how the industry defines quality, how much health equity data the industry has (and how standardized it is), and how organizations conceptualize the financial impact of health inequities on their business. Once there's an incentive to experiment, leaders can better understand how the industry is falling short and identify new ways of delivering care.
- Pessimistic outlook: But there's also a risk that this strategy could default to a "check the box" exercise. Looking to the introduction of HCAHPS scores as an example, there's a risk that organizations start to hyper-focus on specific metrics rather than design holistic strategies to impact the root causes of health inequities. And if entities don't coordinate, provider organizations may face conflicting data gathering requirements that quickly become overwhelming.
Either way, we know that this new strategy won't be a silver bullet. It focuses narrowly on provider organizations, while all stakeholders in the industry play a role in mitigating (or perpetuating) inequities. And a comprehensive health equity strategy has to touch on all three pillars of an equitable health care organization—including the workforce and the community as well as patients.
Your role in advancing health equity starts here
Ultimately, health care leaders can make principled arguments for selecting either path as the right one for them. It boils down to one key indicator: Is your organization ready and able to commit real resources to support this work in the long term?
No matter your answer, every health care organization can still make a meaningful difference in advancing equity. We recommend three strategies that all organizations can and should adopt today. They may or may not map directly to equity metrics within new quality contracts—but they will start to address the underlying causes of inequity.
- Expand your partnership strategy beyond community-based organizations to include all industry players, including competitors. Cross-industry partnerships can create mutual accountability for progress, reduce duplicative efforts, and maximize impact.
- Advocate for policies that address the root causes of inequity—intergenerational poverty and structural racism. Industry leaders can't solve these challenges alone, so ask local, state, and federal policymakers for what you need to make progress more possible, quicker.
- Uplift economic outcomes by adopting an "anchor" approach to hiring and supplying decisions, which includes diverting existing dollars to local economies whenever possible. This development builds a more favorable payer mix, reduces plan membership churn, and strengthens the workforce pipeline.
What each organization does beyond these three elements depends on where it sits in the industry. The most impactful organizations identify their strengths and weaknesses—and find partners who can fill their gaps.
Philips is a health technology company focused on improving people’s lives through meaningful innovation across the health continuum – from healthy living and prevention to diagnosis, treatment, and home care. Applying advanced technologies and deep clinical and consumer insights, Philips partners with customers to deliver integrated solutions that address the Quadruple Aim: improved patient experience, better health outcomes, improved staff experience, and lower cost of care.
This blog post is sponsored by Philips, an Advisory Board member organization. Representatives of Philips helped select the topics and issues addressed. Advisory Board experts wrote the post, maintained final editorial approval, and conducted the underlying research independently and objectively. Advisory Board does not endorse any company, organization, product or brand mentioned herein.

This blog post is sponsored by Philips. Advisory Board experts wrote the post, conducting the underlying research independently and objectively.
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
