Auto logout in seconds.
Continue LogoutVariation in post-discharge quality and costs, as well as related readmissions, makes post-acute care critical to managing an effective episode of care. Through primary research and literature review, the Post-Acute Care Collaborative has identified the preparation for an efficient discharge as a key area that can enhance patient management across the post-acute episode.
In the article below, we review a case study in which an acute care provider extended their care pathway into the post-acute setting through providing a comprehensive care roadmap detailing protocols for a specific population of patients.
To learn about other strategies aimed at facilitating an efficient discharge, download part two of our complete guide on the 10 Keys to an Efficient Post-Acute Episode.
Complimentary Resource: The two main benefits of forming a post-acute care network and how to ensure that you're getting them
Evidence-based care pathways support efficient, high-quality care in the acute space by minimizing variation. To ensure patients continue to receive cost-efficient, high-quality care after discharge, collaborate with PAC providers to adapt existing acute-care protocols to the post-acute setting—and build new pathways that go beyond inpatient treatment and address common challenges to care plan execution in the post-acute setting.
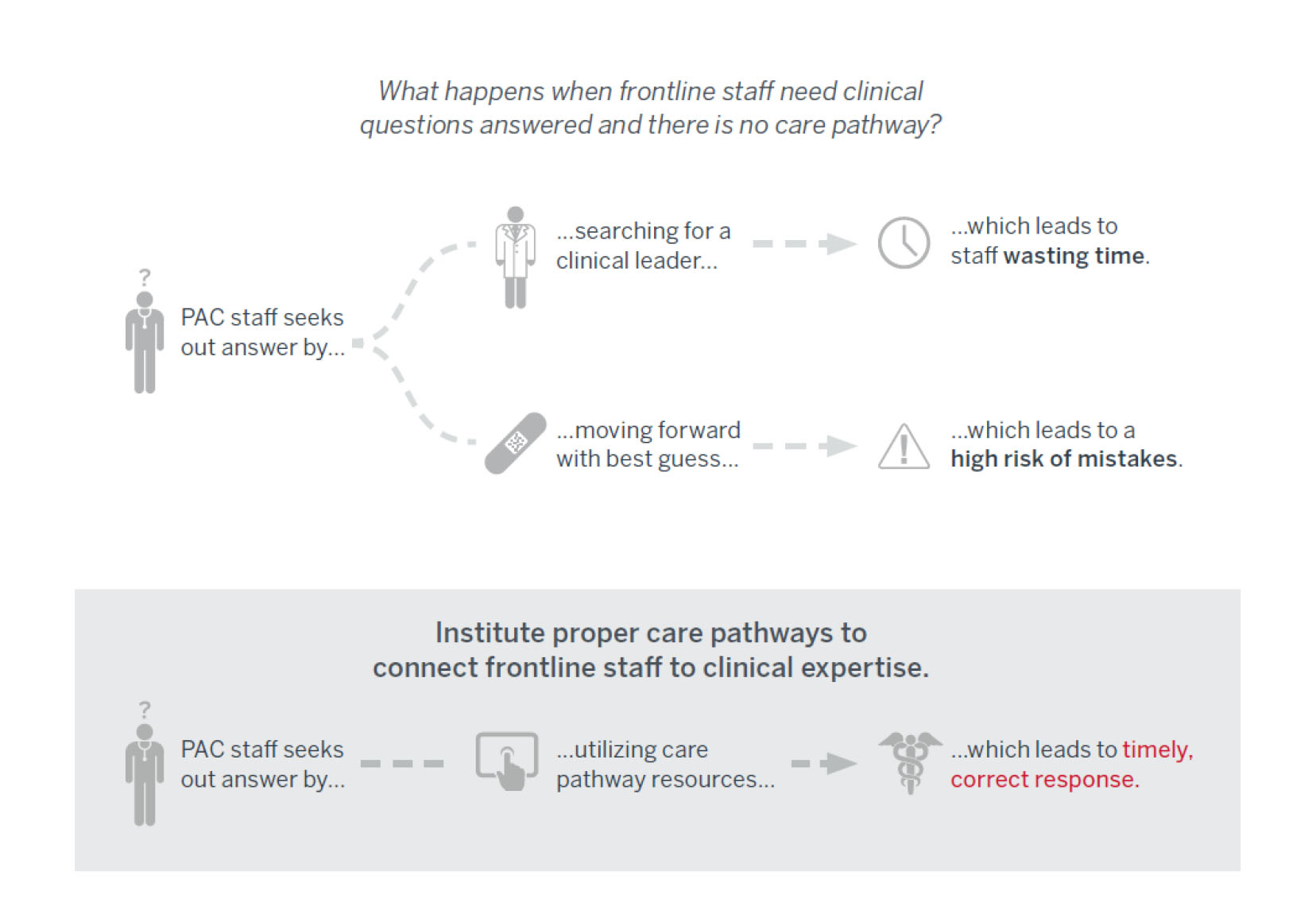
Challenge: Frontline staff in the post-acute setting may be unfamiliar with the expectations hospital staff have regarding a patient’s recovery plan and anticipated timeline, or there may be an unexpected change in a patient’s condition that impacts that plan.
Solution: Create clinician-informed, evidence-based pathways detailing clinical protocols for post-acute care.
Member Spotlight: Care Roadmap Sets the Tone for Treatment Post-Discharge
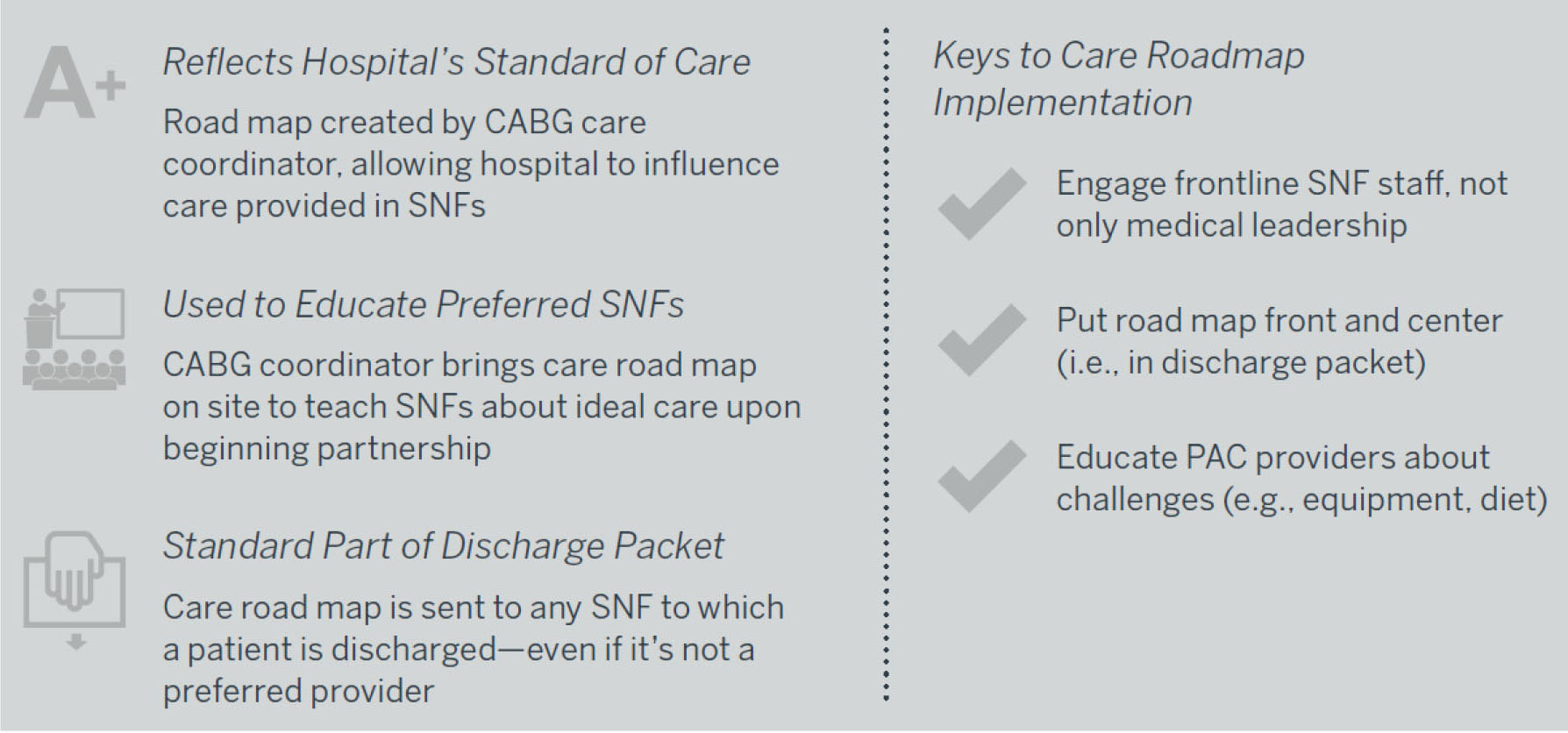
Baystate Medical Center and its partner SNFs have teamed up to reduce costs and prevent readmissions as part of its participation in bundled payments for care improvement (BPCI) for coronary artery bypass graft (CABG) patients. Baystate provides the SNFs with a comprehensive care road map that details post-acute care protocols for CABG patients.
The road map outlines expected care for each day the patient spends in the SNF and lists milestones for discharge. For example, during the first few days, treatment guidelines include incision assessment and dressing changes. Education goals include exercise plans and nutrition counseling. The road map also includes lists of common side effects, as well as instructions for when further intervention may be needed. The care road map is a standard part of the patient’s discharge packet—ensuring it is highly visible for SNF frontline caregivers.
In addition to the road map, Baystate provides additional ongoing support to its partner SNFs. For instance, Baystate’s CABG care coordinator holds education sessions to walk SNF frontline staff through the protocols and answer questions.
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.