Auto logout in seconds.
Continue Logout By Katherine Virkstis, Managing Director and Senior Research Partner
By Katherine Virkstis, Managing Director and Senior Research Partner
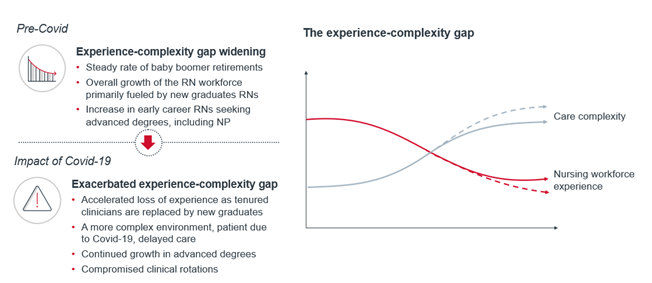
With all the news about critical shortages of nursing staff, one essential issue often gets overlooked in the headlines: the concerning "skills gap." Think of this as a different-in-kind shortage which has been emerging for some time—a shortage of experienced nurses. Covid-19 has exacerbated this challenge, and unless addressed, will threaten patient safety.
Our take: Building a flexible nursing workforce
Prior to the pandemic, there were two forces driving the shortage of nursing experience. The first is the large share of baby boomer nurses who are either reducing their hours or retiring altogether. The other is the explosive growth of new graduate RNs. Between 2001 and 2015, the number of students enrolled in nursing programs more than doubled, increasing from 68,800 to nearly 158,000. This growth has of course been a welcome trend and is in no small part the result of major industry-wide efforts to expand the number of openings for nursing students at colleges and universities. But the collective result of these two forces is a meaningful shift in the age distribution of the nursing workforce. Specifically, there is now a much larger proportion of novice nurses comprising the workforce than a decade ago. And it will likely get worse—as retirement-age nurses leave the workforce, most vacancies created by those departures will be filled by new graduates.
At the same time, care complexity is increasing. Patient acuity continues to rise, especially in the inpatient setting. From 2012 to 2017, the average case mix index for non-ICU patients increased by 0.11, while the number of patients with comorbidities rose and length of stay decreased.
The result of all this is a more novice workforce who must deliver more complex care. The Nursing Executive Center developed a name for this emerging challenge: the experience-complexity gap.
A slower path to competence
The transition to practice is a challenging time for many new graduate RNs. But the emerging experience-complexity gap may be making this transition even more challenging. During our research, many nursing leaders shared a common observation: it is taking longer for nurses to develop clinical competence than previous generations.
Several factors might explain the slower progression from "novice" to "competent." First, there is a growing number of skills and competencies nurses must learn today. Second, it's more difficult to learn new competencies in a faster-paced care environment because there simply isn't as much time to absorb new information and practice new skills. Third, there are a very limited number of less acute, less complicated patients with which new nurses can practice their skills. Finally, there are fewer opportunities for experienced nurses to coach novice nurses, because more complex care delivery occupies a larger portion of their time.
The widening experience-complexity gap, explained
Covid-19 has certainly had an impact on nursing supply and demand, but it's also accelerating pre-existing trends. The collective experience in the nursing workforce is now declining faster because of the pandemic, and care delivery is becoming even more complex. In short: Covid-19 has increased the demand for nurses amid a crisis level workforce shortage, it has also widened the experience-complexity gap.
On the supply side, many nurses are leaving the profession. Reasons include the following: tremendous stress and burnout caused by the pandemic, family caregiving obligations, and early retirement of nurses who choose to hedge their bets and retire now, rather than to remain working in a challenging environment that also poses a new health risk to themselves.
On the demand side, Covid-19 accelerated the rise in care complexity in at least two ways. First, patient needs are more complex. Delays to routine and preventive care result in more advanced needs later. Second, Covid brings a new set of evolving protocols that are challenging for any clinician to stay abreast of, let alone a novice nurse still learning the fundamentals of practice.
Four strategies to close the experience-complexity gap
Advisory Board recommends four actions executives should take to close the widening experience-complexity gap:
- Bolster emotional support and show staff your own vulnerability as a leader
Your best retention strategy right now—for nurses of all tenures—is to offer comprehensive emotional support to mitigate the pandemic's impact on already high levels of stress and burnout. The way you position emotional support is as important as the resources themselves. All leaders must directly address the "I'm fine" attitude of clinicians to convince them to lean on the support you're offering. Do not underestimate the impact your personal vulnerability as a senior leader can have on encouraging nurses to seek needed support. Share the ways in which you are "not fine" because of the pandemic, and how you're prioritizing your own emotional health.
- Dramatically scope the first year of practice
The secret to accelerating the transition to competent practice is ruthless prioritization. Novice nurses can provide safer care if they have full mastery over a small set of skills, rather than a weak grasp on a wide range of skills.
- Differentiate practice for experienced nurses
Create roles that maximize the experience and skills of competent, proficient, and expert RNs. To do so, we recommend staffing models that position competent and proficient nurses "at the hip" of novice nurses. Additionally, staffing models can scale the impact of expert nurses by differentiating their role to leverage their skills and expertise more fully.
One way to differentiate the role of expert nurses is to elevate their responsibilities within the care team. Shift from a staffing model where each nurse carries a similar patient load (regardless of competency level) to one where an expert nurse formally leads a team of less experienced nurses and other support staff.
- Reinforce experienced nurses' identity as system citizens
Experienced nurses' remarkable willingness to flex where, when, and how they work during the pandemic has enabled health systems to quickly expand their Covid-19 capacity. Nurses function as members of a system-wide workforce, which enables leaders to deploy experienced nurses to match variable patient needs across the organization.
Leaders must take advantage of this temporary shift in frontline nurses' perspective and use it to reinforce nurses' identity as system citizens first, and members of their unit or care site second. This shift in identity underpins a system's long-term ability to close the experience-complexity gap by redistributing experienced nurses across the system.
This moment in time represents a critical opportunity for health system leaders. Resist the temptation to "get back to normal." Instead, tap into the experimentation, innovations, and lessons learned during 2020 to accelerate transition to practice, fully leverage the skills and abilities of each member of the care team, withstand continued retirements, and safely meet increasingly complex patient needs. Take stock of what's working well and worthy of system-wide adoption.
The broadening experience-complexity gap is only one of the big challenges nurse leaders are facing in today's staffing environment. To learn more about the hard truths CNOs will need to come to grips with in order to succeed within current and future shortages.
Covid-19 will not fundamentally change nursing supply and demand but it will accelerate pre-existing trends. Collective experience in the nursing workforce will decline faster as a result of the pandemic, and care delivery will become even more complex.
Read on to learn more about the four actions to close the widening experience-complexity gap.
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
