Auto logout in seconds.
Continue LogoutGood news for orthopaedic programs with an outpatient footprint: Advisory Board is forecasting a 44% increase in demand for outpatient joint replacement procedures over the next five years. Capturing that growth, however, requires orthopaedic leaders to make strategic decisions to position their programs to become the top choice among patients, health plans, and referring providers. Moreover, orthopaedic leaders must ensure their programs have the capacity to accommodate volume growth.
There’s no single formula for winning orthopaedic market share. Advisory Board’s past survey shows that patients weigh variables like access, location, provider and facility specialization, recovery time, outcomes, and cost when deciding where to have their joint replacement procedures performed. Anecdotally, we know payers and providers care about similar criteria when influencing referrals. One area that can differentiate an orthopaedic program for all these stakeholders is digital surgery.
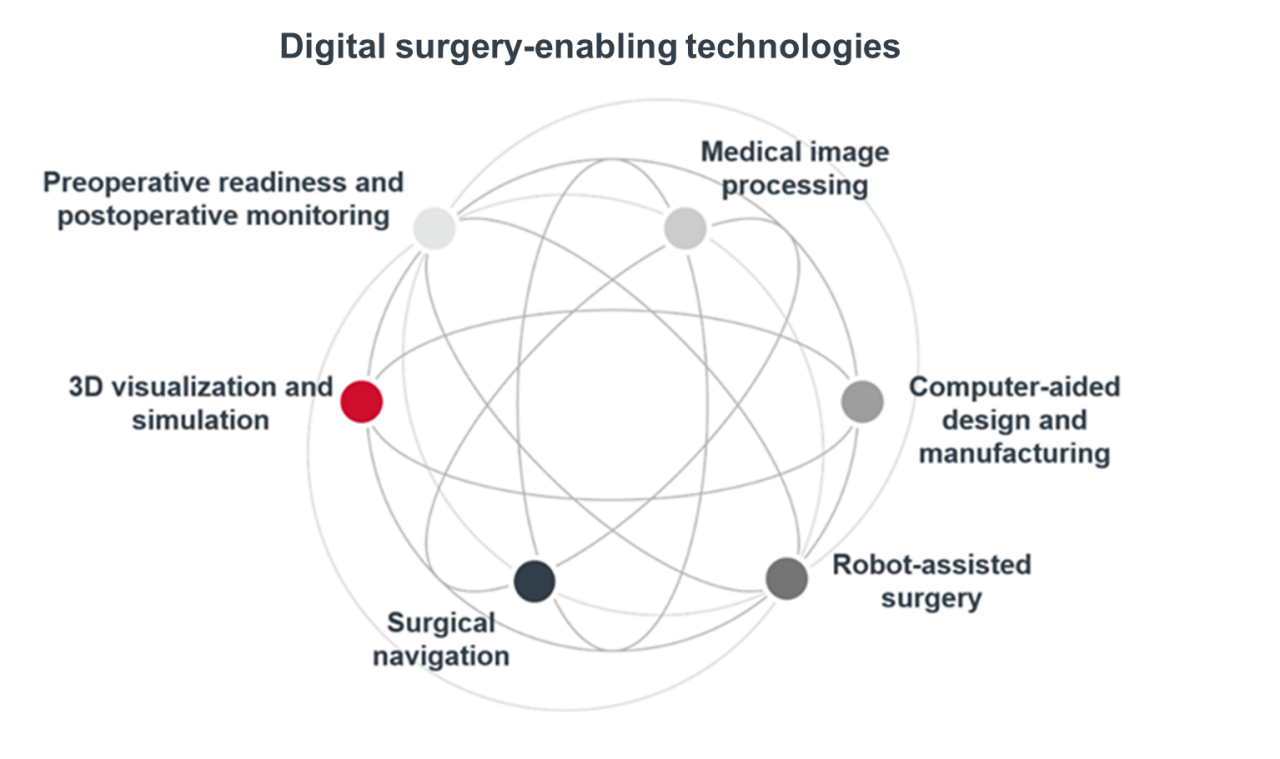
Digital surgery encompasses multiple classes of enabling technologies that facilitate “preoperative planning, surgical performance, therapeutic support, or training.”1 While some digital tools are nascent, data suggests that several have improved clinical outcomes and recovery times, while others increase program capacity and access. For example, one study found that an orthopaedic AI tool that processes CT data to make measurements can reduce total time spent per case by an average of 94%.2
While the number of surgeries performed using surgical robotics is expected to grow at a compound annual growth rate of 10.5% in the U.S. from 2020 to 2030, digitally enabled surgery can still be a differentiator in orthopaedic offerings today.3 Here are three ways digital surgery can help prime orthopaedic programs for growth.
1. Greater access and availability
Time is of the essence — particularly for baby boomers and younger patients who want to return to active lifestyles quickly. Orthopaedic programs can set themselves apart from other in-network options based on time to next available appointment. Digital solutions can help programs navigate shifting sites of care and shave time off procedures and planning without compromising results, leading to greater (and more predictable) program capacity.
For example, Dr. Cody Wyles, an orthopaedic surgeon at Mayo Clinic, has found in a study that AI-enabled imaging can document a hip cup’s position more quickly and accurately than a human can.4 His team’s AI application processed 15,000 patients’ data in eight hours — a time savings of two to three months over manual processing. This kind of time savings allows clinicians to see more patients and improve timely access.
In a meta-analysis, patients who had robotic-assisted total knee arthroplasty (TKA) had a 14% shorter length of stay than patients receiving conventional TKA, leading to faster bed turnover and expanded capacity.5
2. Improved procedural results
Before and during procedures, surgeons can employ digital solutions to enhance patient outcomes. Imaging techniques and real-time navigation systems can optimize surgical planning and execution, leading to better physician precision and accuracy. For instance, digital fluoroscopic navigation improves accuracy in direct anterior approach total hip arthroplasty (THA) over unaided standard fluoroscopy: 66% (versus 40%) of patients who underwent THA with digital fluoroscopic navigation had less than three millimeters of leg length discrepancy.6 Similarly, the use of robotic-assisted surgical tools can improve procedural outcomes: one study found a lower incidence of patellar tilt (a significant contributing factor for revision TKA) in a robotic-assisted TKA cohort compared to in manual TKA.7
While technology can’t compensate for experience or technique, tools like digital fluoroscopy and robotic-assisted technologies that can help surgeons improve their accuracy. This in turn can reduce the risk of complications, boost patient satisfaction, enhance procedural accuracy, and help practices differentiate themselves.
3. Better downstream outcomes
By increasing accuracy, digital surgery can reduce the need for future surgeries and minimize rates of revision surgeries and readmission, which is appealing to patients, payers, and referring providers. For example, patients who used digital fluoroscopy had 30% and 36% lower 90- and 365-day, hip-related readmission rates, respectively, than patients who underwent manual THA.8
Digital tools may also help reduce patient pain and improve patient satisfaction compared to non-digital surgery. Of course, not all studies have demonstrated consistent outcomes. However, one study found that two weeks postoperatively, patients undergoing robotic-assisted TKA had a lower average visual analogue scale (VAS) pain score at rest and with activity than the manual instrumentation group.9 Another study shows lower morphine use by patients who underwent robotic-assisted TKA compared to patients who underwent manual TKA.10 And a third study demonstrates that patients in the robotic-assisted TKA had a better average satisfaction score of 7.1, compared to a score of 6.6 for patients in the manual TKA group.11
Digital innovation spotlight: VELYSTM Enabling Tech
Johnson & Johnson’s VELYSTM Enabling Technology is a portfolio of technologies that support orthopaedic surgery techniques through real-time data and clinical insights. VELYSTM Robotic-Assisted Solution and VELYSTM Hip Navigation are two platforms, and they have been proven to show the value of digital surgery outlined above.12, 13
For example, VELYSTM Robotic-Assisted Solution, which has shown that it can be adopted efficiently with a short learning curve, has demonstrated to improve downstream outcomes.14, 15, 16 In one study, it reduced knee-related hospital revisits by 45% and knee-related readmissions by 53% compared to patients receiving manual TKA.17 It also improved VAS pain scores, knee function, and patient-reported outcomes post-surgery compared to patients receiving surgical navigation.18
VELYSTM Hip Navigation can also help distinguish an orthopaedic program by enhancing predictability and efficiency, thus facilitating patient access. One study showed that VELYSTM Hip Navigation reduced operating room time by an average of 33% compared to procedures using fluoroscopy and conventional overlay technique.19 It also has been shown to improve mean overall cup positioning success by 19% compared to manual THA, thus helping to improve a program’s procedural outcomes.20
Considerations for orthopaedic leaders
Digital surgery is one of many offerings that can help an orthopaedic program stand out by improving access, procedural results, and downstream outcomes for patients. While we expect digital surgery volumes to continue growing, digital enabling technologies may not be the right answer for all orthopaedic programs. Here are some considerations to weigh for any new technology investment:
- Does this investment support my top program goals?
- Can I make a business case to justify the investment? Am I accounting for direct revenue as well as indirect returns (such as growth or savings enabled by expanded capacity, easier physician recruitment, and leverage in health plan negotiations)?
- What is the learning curve associated with adopting this new software? What support will the vendor provide with training and licensing requirements? Do I anticipate physician hesitation or lack of trust in the new technology?
- How will this new tool impact my current physical space, staffing, and scheduling protocols?
- Does this tool meet my organization’s cybersecurity and interoperability requirements?
- What health equity impacts could this investment have? What patient populations were included in the tool’s design and testing?
To help capture growth and compete for market share, orthopaedic leaders can consider making investments in digital surgery to help differentiate their program. Platforms such as VELYSTM Robotic-Assisted Solution and VELYSTM Hip Navigation can improve access to joint replacements, procedural results, and downstream outcomes. Thus, they can help orthopaedic programs better appeal to patients, health plans, and providers.
1 Raza MM, Venkatesh KP, Diao JA, et al. Defining digital surgery for the future. NPJ Digital Medicine. October 19, 2022.
2 James J and Genc K. Using AI to improve patient-specific orthopedic workflows. Orthopedic Design & Technology. February 15, 2022.
3 Top robotic surgery companies to follow in 2023. Strategic Market Research. August 2023.
4 Mayo Clinic lab looks to impact orthopedics through artificial intelligence tools. Mayo Foundation for Medical Education and Research. April 2023.
5 Hoeffel D, Goldstein, Intwala D, et al. Systematic review and meta-analysis of economic and healthcare resource utilization outcomes for robotic versus manual total knee arthroplasty. Journal of Robotic Surgery. October 11, 2023.
6 O’Leary R, Saxena A, Arguelles W, et al. Digital fluoroscopic navigation for limb length restoration during anterior total hip arthroplasty. Arthroplasty Today. October 11, 2022.
7 Severson EP, Musto M, Lewandowski TM, et al. Improved Patellar Tracking in Image-Free Robotic-Assisted Total Knee Arthroplasty. Mid-America Orthopaedic Association 40th Annual Meeting; Miramar Beach, FL 2023.
8 Hamilton WG, Sershon RA, Gupta A, et al. Readmission rate and healthcare utilization outcomes of computer-assisted fluoroscopy-based hip navigation versus manual total hip arthroplasty. Expert Review of Medical Devices. July 25, 2023.
9 Bhimani SJ, Bhimani R, Smith A, et al. Robotic-assisted total knee arthroplasty demonstrates decreased postoperative pain and opioid usage compared to conventional total knee arthroplasty. Bone & Joint Open. October 27, 2020.
10 Severson EP, Lewandowski TM, Fleming MF, et al., Resource Utilization with Robotic and Manual Total Knee Arthroplasty in the Critical Access Hospital Setting. Mid-America Orthopaedic Association 40th Annual Meeting; Miramar Beach, FL 2023.
11 Smith AF, Eccles CJ, Bhimani SJ, et al. Improved patient satisfaction following robotic-assisted total knee arthroplasty. The Journal of Knee Surgery. June 2021.
12 Fawley D, Bernard T, Morrison JC, Redmond J. Cup Positioning Accuracy of Direct Anterior Approach Using a Non-Invasive, Image-Based Software Navigation System in Primary Total Hip Arthroplasty. Podium Presentation, ISTA 2023 Annual Congress; September 27-30, 2023; New York, NY.
13 VELYSTM Robotic-Assisted Solution Value Analysis Brief. DePuy Synthes. 2024.
14 Lall JS, McLennan AL, et al., Learning Curve for VELYSTM Robotic-Assisted TKA system. Orthopaedic Research Society Annual Meeting; Dallas, TX 2023.
15 Morrisey ZS, Barra MF, Guirguis PG, et al., Transition to robotic total knee arthroplasty with kinetic alignment is associated with a short learning curve and similar acute-period functional recoveries. Cureus. May 11, 2023.
16 Pagen C, Karasavvidis T, DeCook C, et al., The Learning Curve in Robotic-Assisted Total Knee Arthroplasty: A Single Surgeon Cohort. Current Concepts in Joint Replacement; Orlando, FL 2022.
17 Huang P, Cross M, et al. Early Clinical and Economic Outcomes of VELYSTM Robotic-Assisted Solution (VRAS) Compared to Manual Total Knee Arthroplasty. Presented at Computer Assisted Orthopedic Surgery 2024, June 19-22, 2024; Groningen, The Netherlands.
18 Clatworthy M. Patient-specific TKA with the VELYSTM Robotic-Assisted Solution. Surgical TechnologyInternational. May 19, 2022.
19 Goodell P, Ellis S, Kokobun B, et al. Computer navigation vs. conventional overlay methods in direct anterior total hip arthroplasty: A single surgeon experience. Cureus. October 2022.
20 Fawley D, Bernard T, Morrison JC, Redmond J. Cup Positioning Accuracy of Direct Anterior Approach Using a Non-Invasive, Image-Based Software Navigation System in Primary Total Hip Arthroplasty. Podium Presentation, ISTA 2023 Annual Congress; September 27-30, 2023; New York, NY.
DePuy Synthes is the orthopaedics company of Johnson & Johnson. With one of the most comprehensive orthopaedics portfolios in the world, we help heal and restore movement for millions of patients. Our products span various specialties, including joint reconstruction, trauma, craniomaxillofacial, spinal surgery, and sports medicine.
Building on our proud legacy of industry firsts, we are honoring our commitments to quality and innovation while creating a future where it's easier than ever before to keep people moving.
Learn more about DePuy Synthes.
This report is sponsored by DePuy Synthes, an Advisory Board member organization. Representatives of DePuy Synthes helped select the topics and issues addressed. Advisory Board experts wrote the report, maintained final editorial approval, and conducted the underlying research independently and objectively. Advisory Board does not endorse any company, organization, product or brand mentioned herein.
To learn more, view our editorial guidelines.

This article is sponsored by DePuy Synthes, the orthopaedics company of Johnson & Johnson. Advisory Board experts wrote the report, maintained final editorial approval, and conducted the underlying research independently and objectively.
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.



